Vestibular Schwannoma Presenting with Bilateral Papilledema Without Hydrocephalus: Case Study
Authors: Carlos Candanedo, Samuel Moscovici, Joshua M. Kruger, Cezar J. Mizrachi, Ruth Eliahou, Sergey Spektor
- Neurosurgery, Hadassah-Hebrew University Medical Center
- Ophthalmology, Hadassah-Hebrew University Medical Center
- Radiology, Hadassah-Hebrew University Medical Center
- Department of Neurosurgery, Hadassah Hebrew University Hospital
Corresponding Author: Sergey Spektor, sergeyspektor@gmail.com
Disclosures can be found in Additional Information at the end of the article.
Abstract
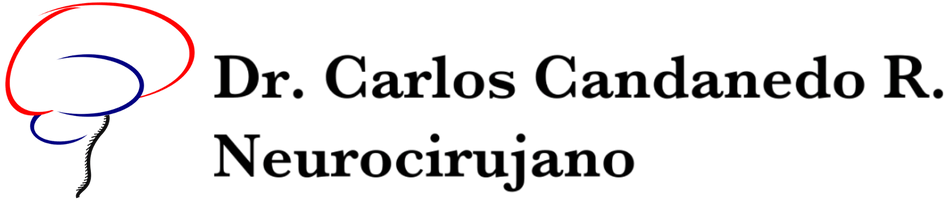
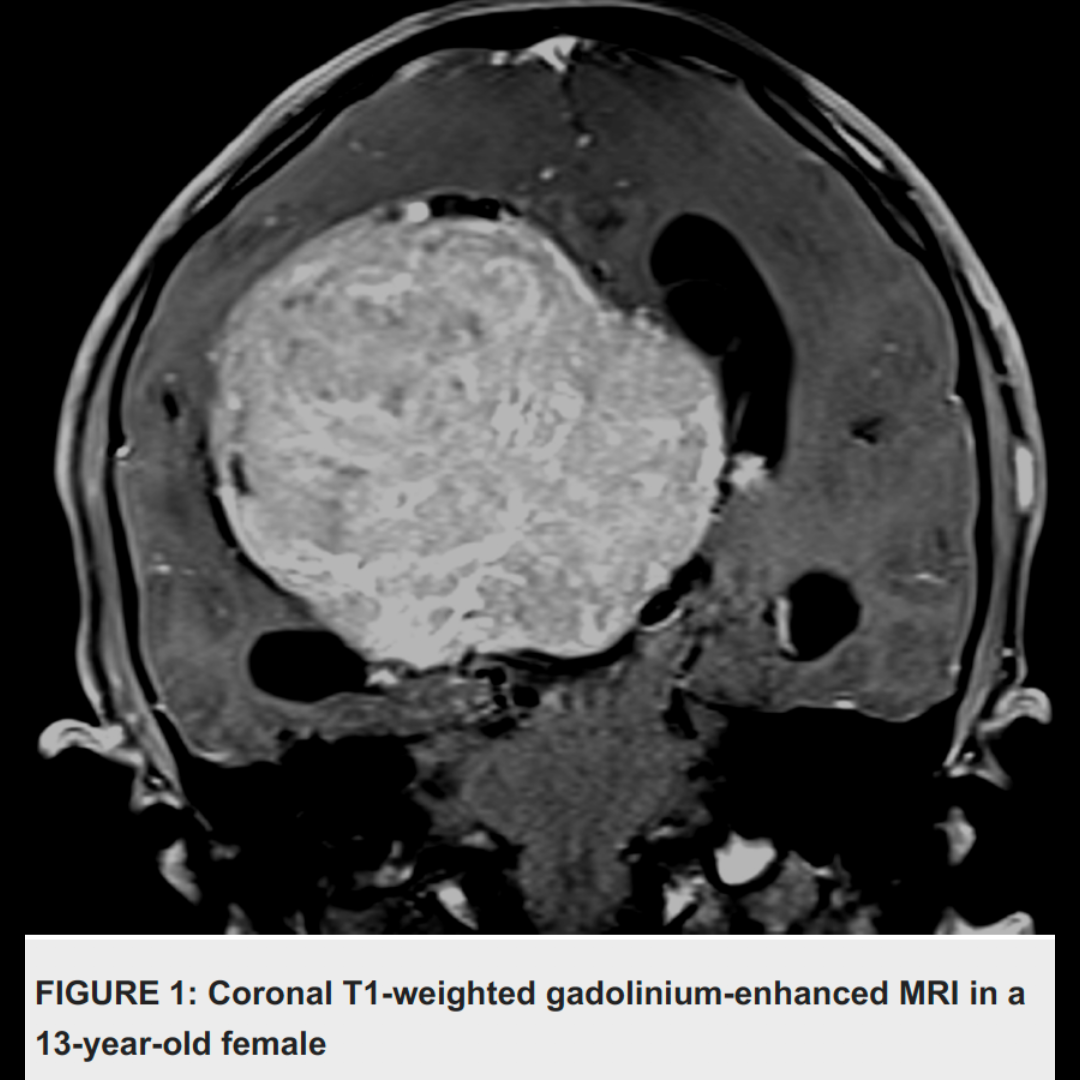
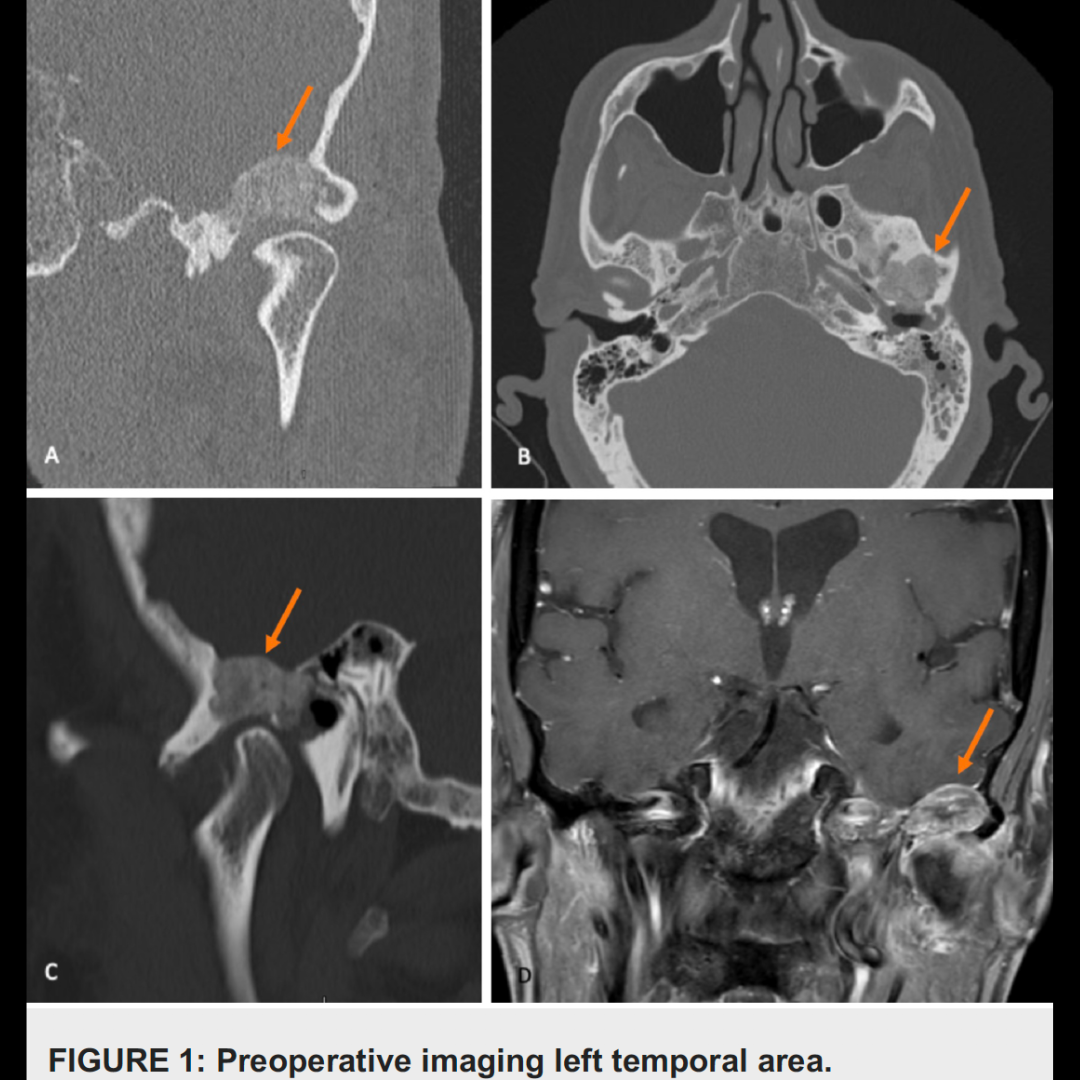
Bilateral papilledema secondary to obstructive or communicating hydrocephalus in patients with vestibular schwannomas is a known presentation; however, papilledema in the absence of hydrocephalus is rarely reported and its mechanism is poorly understood. We report a case of a 20-year-old woman presenting with visual deterioration and bilateral papilledema on fundoscopy. Magnetic resonance imaging (MRI) revealed a giant vestibular schwannoma with no sign of hydrocephalus.
The only imaging evidence of increased pressure on preoperative imaging studies was seen on a T2-weighted MRI, where there was subtle dilatation of the arachnoid space of the optic sleeve. We presume that this patient developed papilledema by some mechanism not connected to hydrocephalus. In a young patient, papilledema may be a sign preceding hydrocephalus, or she may have had pseudotumor cerebri concomitant with her vestibular schwannoma.
In either case, removal of the vestibular schwannoma solved the problem. She had complete visual recovery, irrespective of the mechanism.