Intervening in the Acute Phase of Postradiation Carotid Blowout Syndrome
Marrigje A. de Jong¹, Carlos Candanedo², Menachem Gross¹, José E. Cohen²,³
¹Department of Otolaryngology/Head and Neck Surgery, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
²Department of Neurosurgery, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
³Division of Endovascular Neurosurgery and Interventional Neuroradiology, Hadassah-Hebrew University Medical Center, Jerusalem, Israel
Int Arch Otorhinolaryngol 2019;23:172–177.
Address for correspondence: Dr. Marrigje A. de Jong, MD, Department of Otolaryngology/Head and Neck Surgery, Hadassah Hebrew University Medical Center, Jerusalem, 91120, Israel (e-mail: dejong.marije@gmail.com).
Abstract
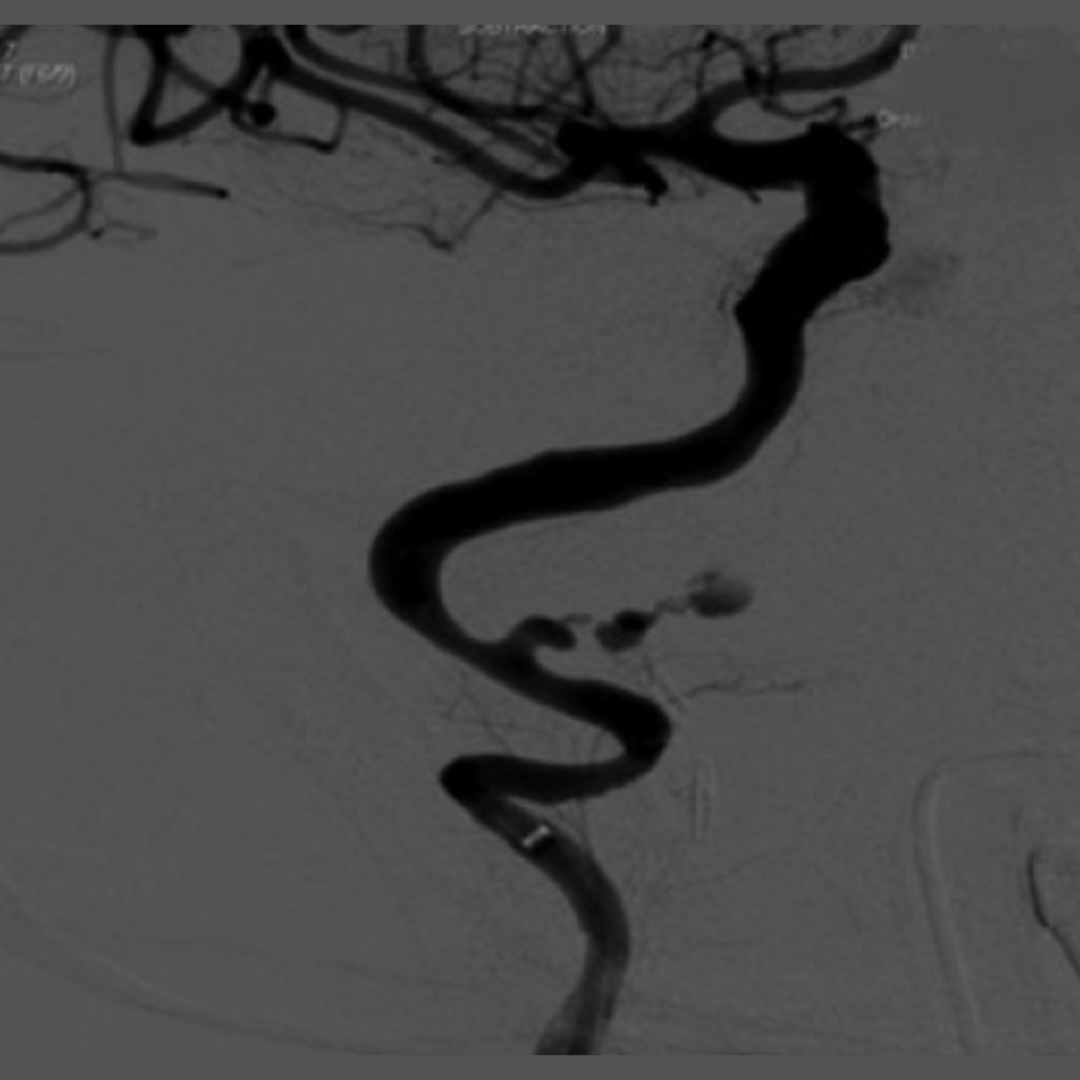
Introduction: Acute carotid blowout syndrome (aCBS) is a severe complication of head and neck cancer (HNC). It can be defined as a rupture of the extracranial carotid arteries, or one of their branches, that causes life-threatening hemorrhage, and which nowadays can be treated with urgent endovascular intervention.
Objective: We retrospectively evaluate the endovascular management of aCBS and its outcome in years of survival.
Methods: Retrospectively, we describe our experience with endovascular control of aCBS in patients treated for HNC. We review the characteristics, pathology, endovascular treatment, and morbidity and assess the gain in life years.
Results: Nine individuals were included in this study. Four patients had been previously diagnosed with laryngeal squamous cell carcinoma (SCC), one with paranasal SCC, one with nasopharyngeal carcinoma, and three with oral or maxillary adenocarcinoma. All subjects underwent radiotherapy and surgical excision to different extents. Twelve endovascular procedures were performed for injuries to the internal carotid artery (n = 3; 25%), external carotid artery (n = 1; 7%), or one of their branches (n = 8; 67%). Deconstructive methods were used in nine procedures, and three procedures were mainly reconstructive with deployment of covered stents. Total control of bleeding was achieved in all individuals with no intraprocedural complications.
Conclusion: Endovascular therapy is an effective alternative for the management of exsanguinating CBS. In our series, this palliative therapy increased the overall patient survival by an estimated 9 months.