Middle Cerebral Artery (M3) Aneurysm: Growing Dissecting Opercular Middle Cerebral Artery Aneurysm, Coil Occlusion of the Precentral Artery with a Low-Profile Microcatheter Under Local Anesthesia, Provocative Test for Neurological Monitoring, Parent Artery and Aneurysm Occlusion, and Excellent Clinical Outcome
Jose´ E. Cohen, John Moshe Gomori, Carlos Candanedo, Samuel Moscovici, and Gustavo Rajz
Abstract
Aneurysms distal to the middle cerebral artery (MCA) bifurcation are infrequent, comprising only 1–7% of all MCA aneurysms. Rather than originating solely from hemodynamic causes, these distal aneurysms are commonly secondary to other etiologies, including infectious emboli caused by subacute endocarditis, vasculitis, tumor emboli, brain trauma, or dissection.
Open surgery is the classical treatment for these aneurysms, with treatment strategies that include aneurysm clipping, aneurysm trapping, and aneurysm trapping plus bypass. The main difficulty with surgery is the precise surgical localization of small M3–M4 aneurysms. Inaccurate localization of these vascular lesions may result in larger craniotomies and unnecessary arachnoid and pial dissections, in some cases with permanent neurological injury.
Endovascular alternatives present a number of challenges because of the distant, small, and tortuous route. In addition, for peripheral MCA aneurysms, parent arteries are usually difficult to preserve.
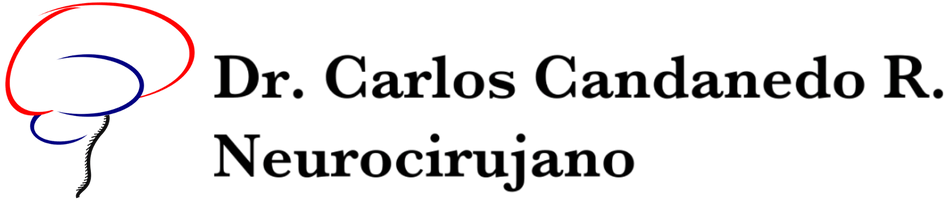
We present the case of a 65-year-old woman with an unremarkable medical history except for heavy smoking and arterial hypertension, who consulted after a first-ever transient episode of speech alterations. A left hemispheric transient ischemic attack was diagnosed based on her neurological evaluation in the Emergency Department. MRI confirmed the presence of two distal left MCA aneurysms. Diagnostic angiography confirmed a midsize insular aneurysm of the superior branch of the MCA and a second, more peripheral and larger aneurysm affecting the opercular segment of a tortuous precentral artery. The parent artery presented a focal severe arterial narrowing proximal to the aneurysm.
The patient was managed with aspirin and statin therapy and recommended neuroradiological follow-up. Transthoracic and transesophageal echocardiogram showed no valvular disease or intracavitary tumor. The patient remained clinically stable. However, diagnostic angiography obtained after 6 months confirmed enlargement of the M3 aneurysm, and therapy was proposed.
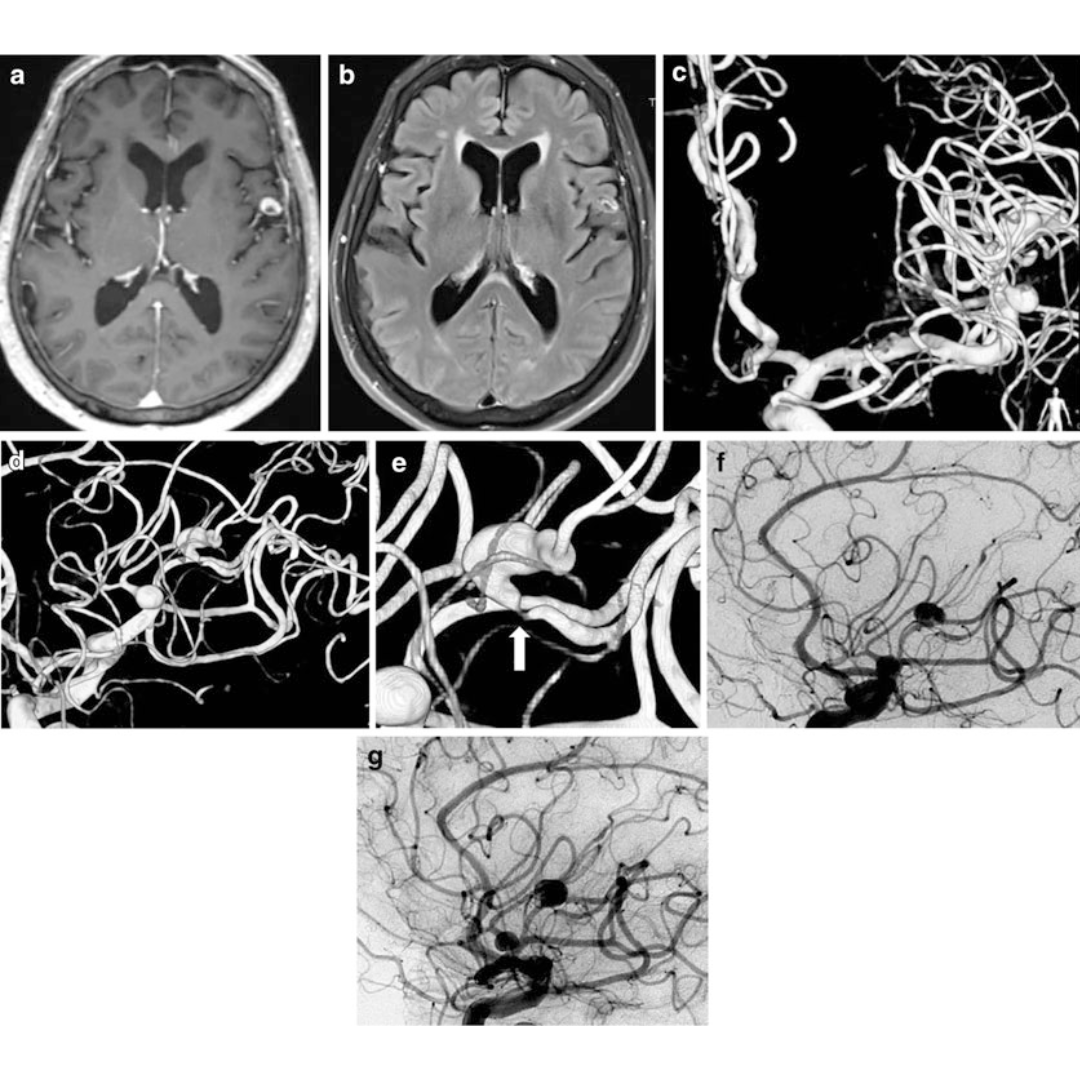
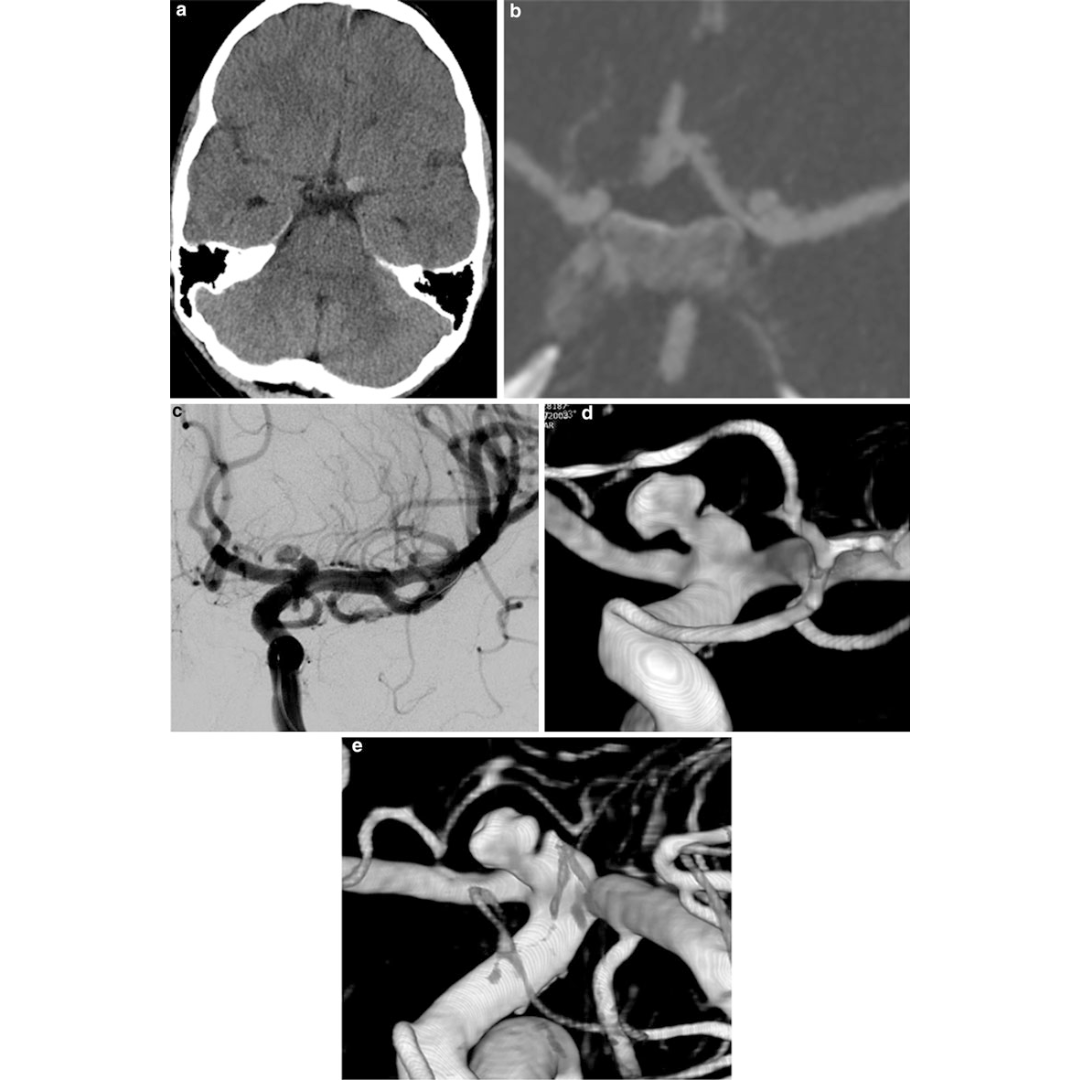
Under local anesthesia, the parent artery was navigated with a Marathon microcatheter and occluded with a detachable coil at the stenosis immediately proximal to the aneurysm origin, with special care not to jeopardize distal leptomeningeal anastomoses. There were no clinical complications. The patient was discharged after 2 days without a neurological deficit. Angiographic follow-up confirmed complete occlusion of the treated aneurysm. Cranial MRI showed no signs of cortical ischemia.
This case illustrates an uncommon and probably underdiagnosed group of distal MCA aneurysms, usually treated surgically, that can be managed by parent artery occlusion with endovascular means. This case also demonstrates the use of a low-profile microcatheter to deploy compatible detachable microcoils that allowed a precise, controlled, and potentially reversible occlusion. The endovascular treatment of distal MCA aneurysms is the main topic of this chapter.