Impact of Extent of Resection and Adjuvant Radiation Therapy in Progression-Free Survival in Patients with Spheno-Orbital Meningioma
Samuel Moscovici, Andrew H. Kaye, Carlos Candanedo, José E. Cohen, Yigal Shoshan, Sergey Spektor
Department of Neurosurgery, Hadassah Hebrew University Medical Center, Jerusalem, Israel
Assuta Hospital, Tel Aviv, Israel
Article Info
Keywords:
Spheno-orbital meningioma, Hyperostosis, Proptosis, Skull base, Radiosurgery, Optic nerve
Abstract
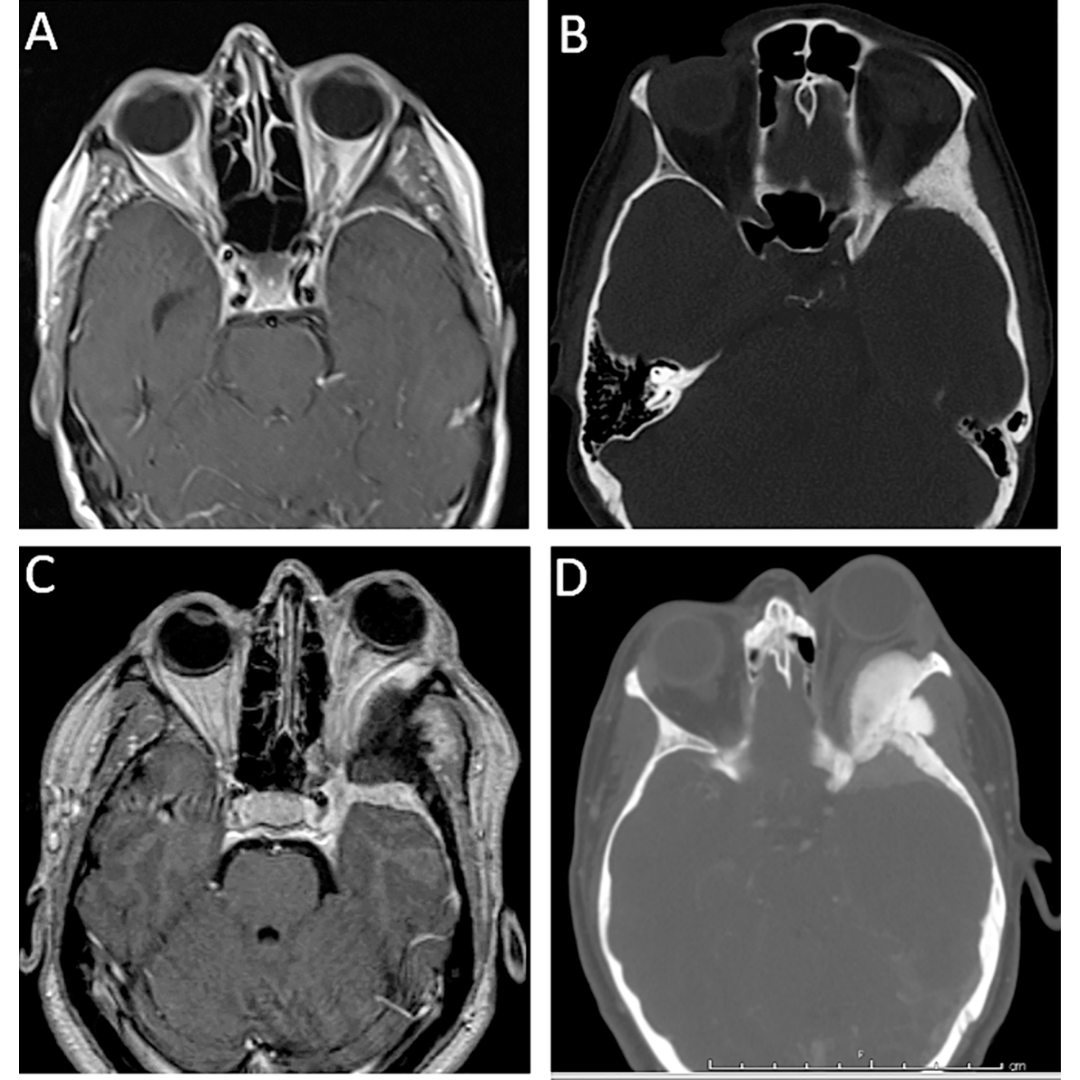
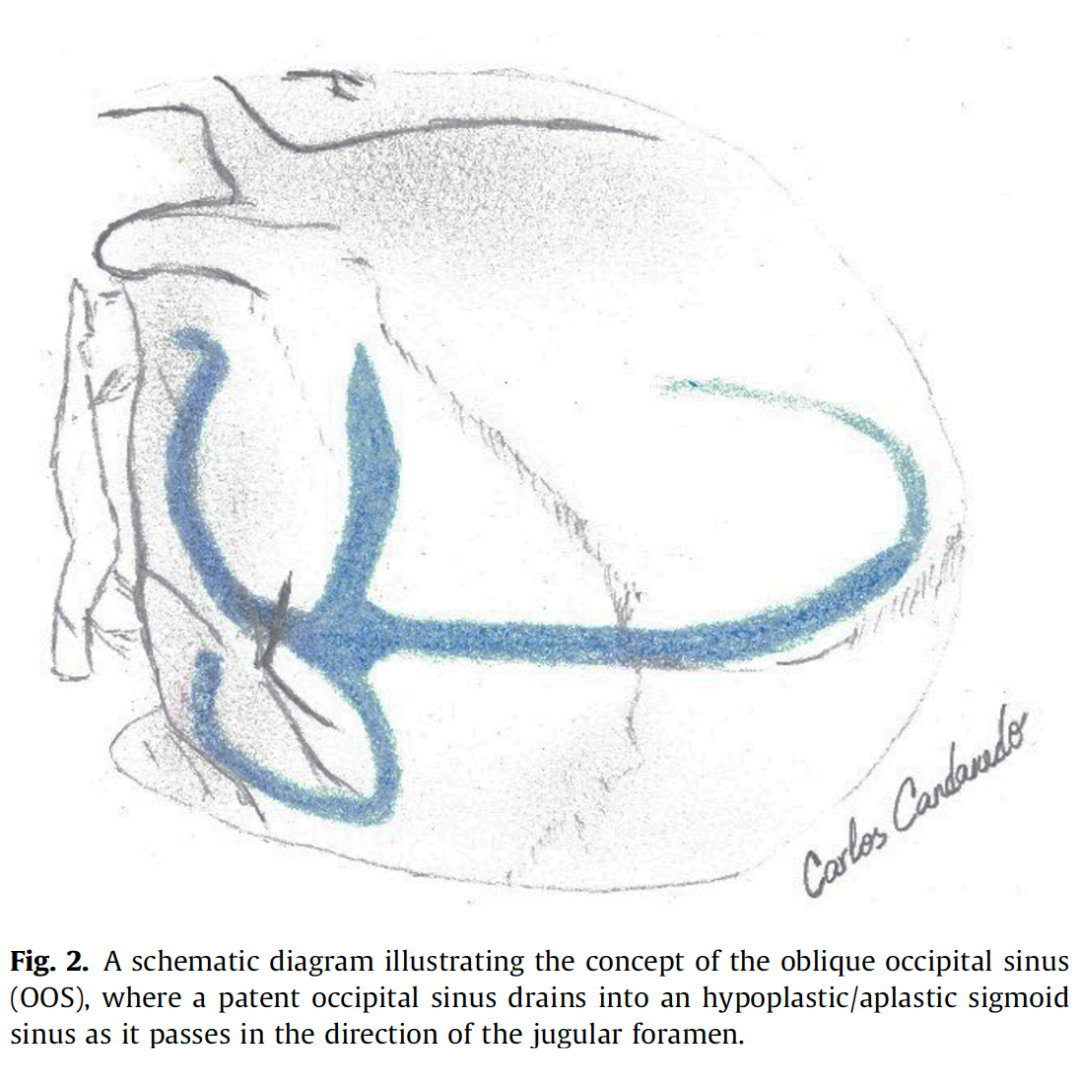
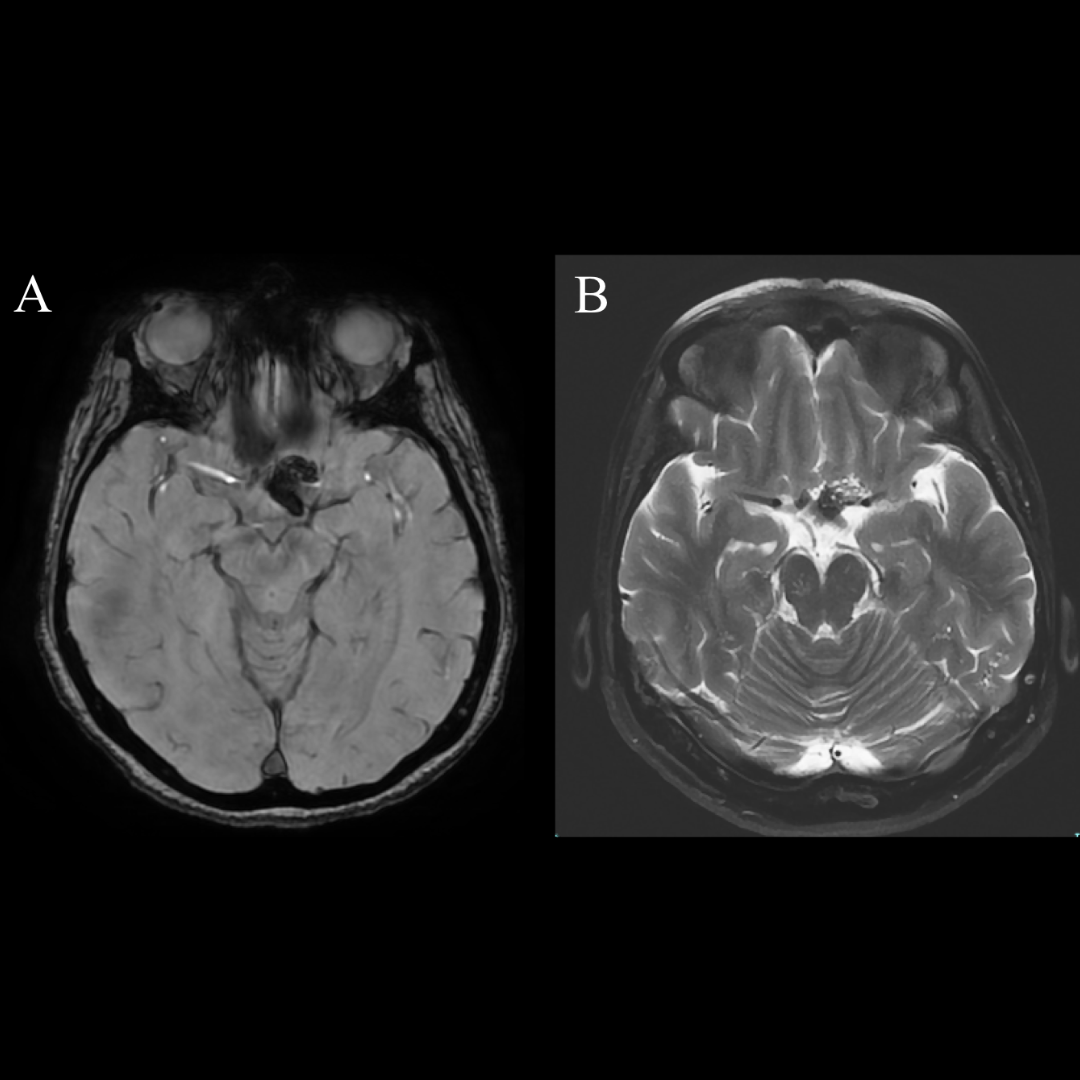
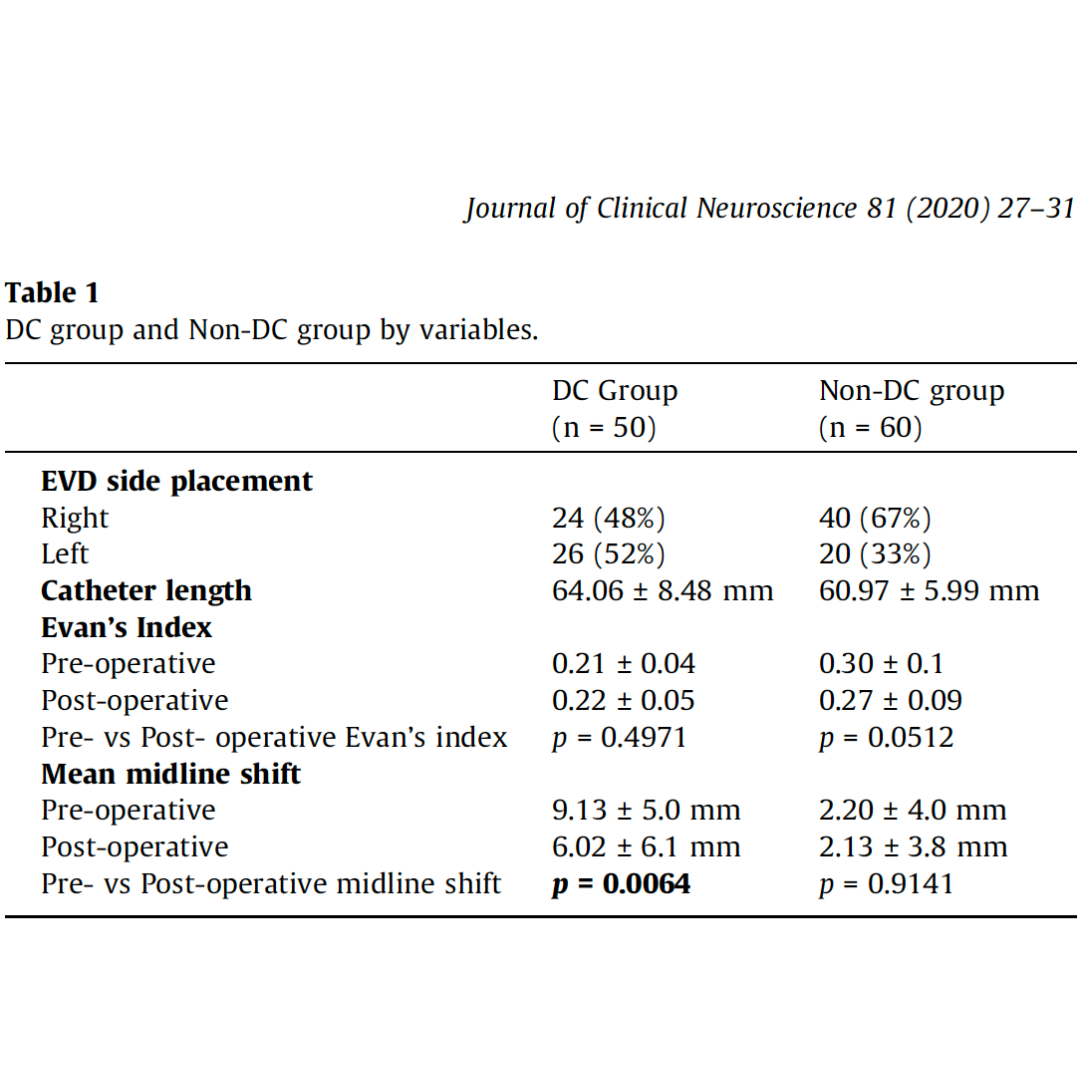
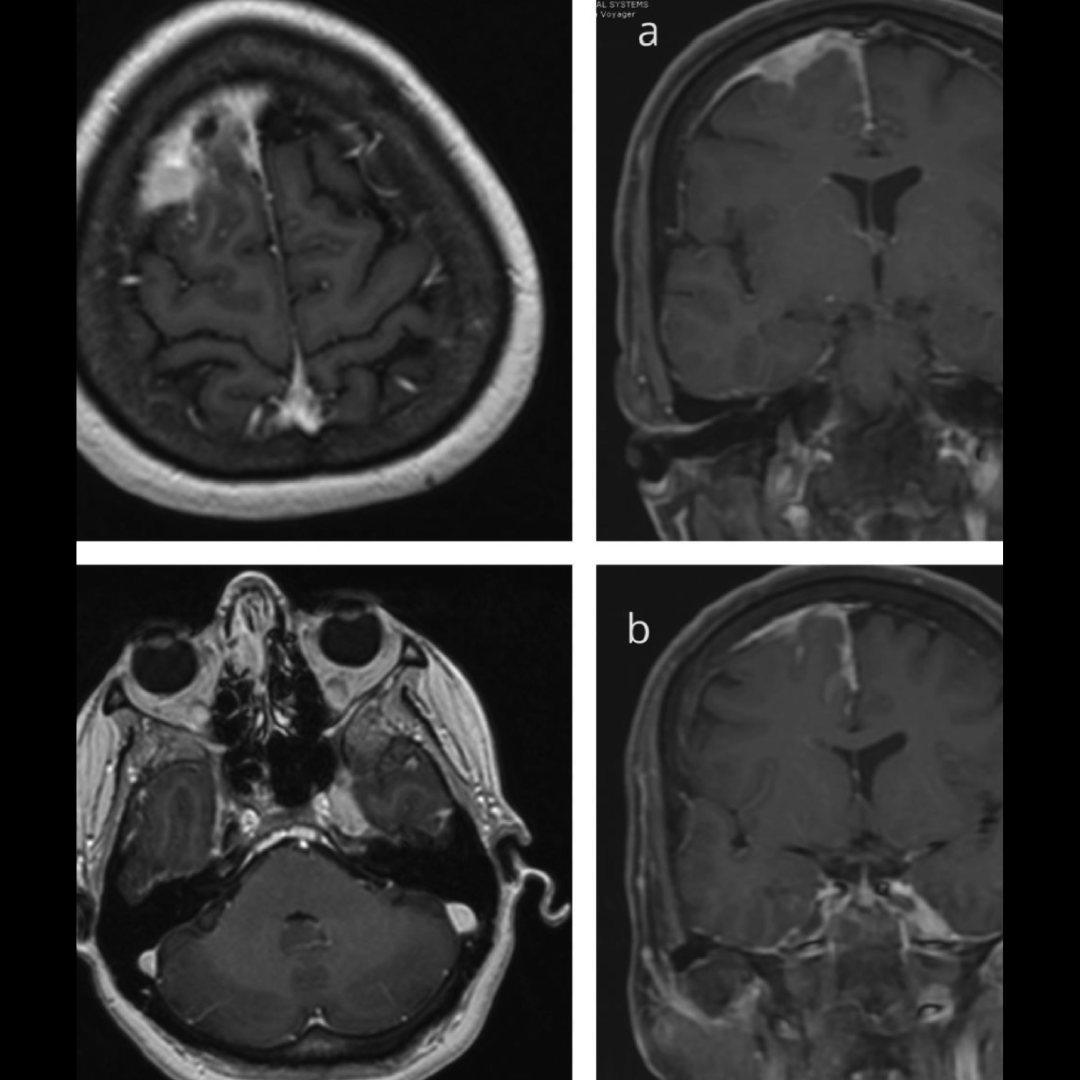
Background: Spheno-orbital meningiomas (SOM) are known to invade critical skull base areas. The authors report a series of WHO I SOM, propose a subclassification of this tumor according to its extension to critical positions, and analyze the impact of the extent of resection and the role of stereotactic radiotherapy in tumor recurrence.
Methods: A prospective maintained university medical center registry was utilized to undertake a retrospective review of patients operated with WHO I SOM. Details related to the critical skull base regions’ extension (superior orbital fissure, cavernous sinus, orbital apex), extent of resection, and adjuvant radiosurgery were collected. Statistical calculations were performed using IBM SPSS Statistics version 25. A p-value < 0.05 was considered significant. Survival analysis was performed using Kaplan-Meier survival analysis and the log-rank test.
Results: A total of 77 patients operated from 2002 to 2021 were included. There were 65 women (84.4%) and 12 men (15.6%). The mean age at surgery was 54.8 years (median 53 years, range 23–88). Tumors were defined as local in 28 (35.4%) and with extension into the skull base critical structures in 51 (64.6%). Gross total resection (GTR) was achieved in 35 (44.3%), subtotal resection (STR) in 40 (50.6%), and partial resection (PR) in four (5.1%). Surgical morbidity was 10%. There was no surgical mortality. 28 patients with STR or PR were treated with adjuvant radiotherapy. The total length of follow-up was a mean of 172.3 months. There were 14 recurrences/progressive growths (17.7%), 63 patients (79.7%) had no recurrence/progressive growth, and two patients (2.5%) were lost to follow-up. Progression-free survival (PFS) was significantly different in patients with invasive tumors, in whom the extent of resection was subtotal, with a longer PFS in patients who were treated with adjuvant radiotherapy (p-value < 0.001).
Conclusions: SOM could be divided into two groups according to its skull base extension, facilitating decision management and outcome prediction. Patients with local WHO I SOM had a higher rate of GTR and better PFS than tumors extending to involve critical regions. When STR or PR is achieved, postoperative adjuvant radiotherapy is advised if there is evidence of previous tumor growth.