Solid vs. Cystic Predominance in Posterior Fossa Hemangioblastomas: Implications for Cerebrovascular Risks and Patient Outcome
Samuel Moscovici, Carlos Candanedo, Sergey Spektor, José E. Cohen, Andrew H. Kaye
Received: 22 December 2020 / Accepted: 23 March 2021
The Author(s), under exclusive license to Springer-Verlag GmbH Austria, part of Springer Nature 2021
Abstract
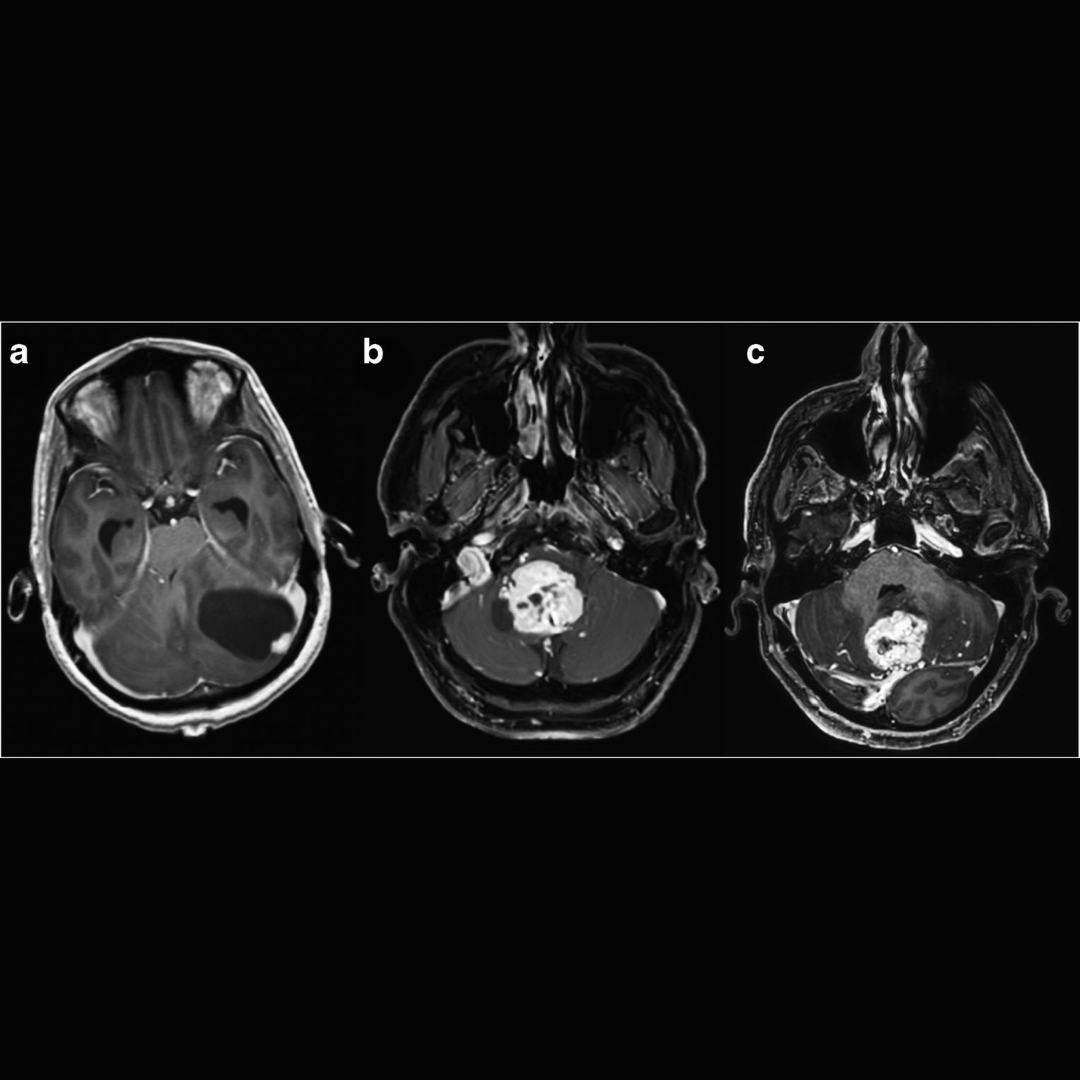
Background: Hemangioblastomas (HGBs) are highly vascular benign tumors, commonly located in the posterior fossa, with 80% being sporadic. Patients typically present with features of raised intracranial pressure and cerebellar symptoms. HGB can be classified as either mostly cystic or solid. Although the solid component is highly vascularized, aneurysm or hemorrhagic presentations are rarely described, but when they do occur, they can have catastrophic results.
Methods: We identified 32 consecutive patients with posterior fossa HGB who underwent surgery from 2008 through 2020 at our medical center. Tumors were classified as predominantly cystic or solid according to radiological features. Resection was defined as gross total resection (GTR) or subtotal resection (STR).
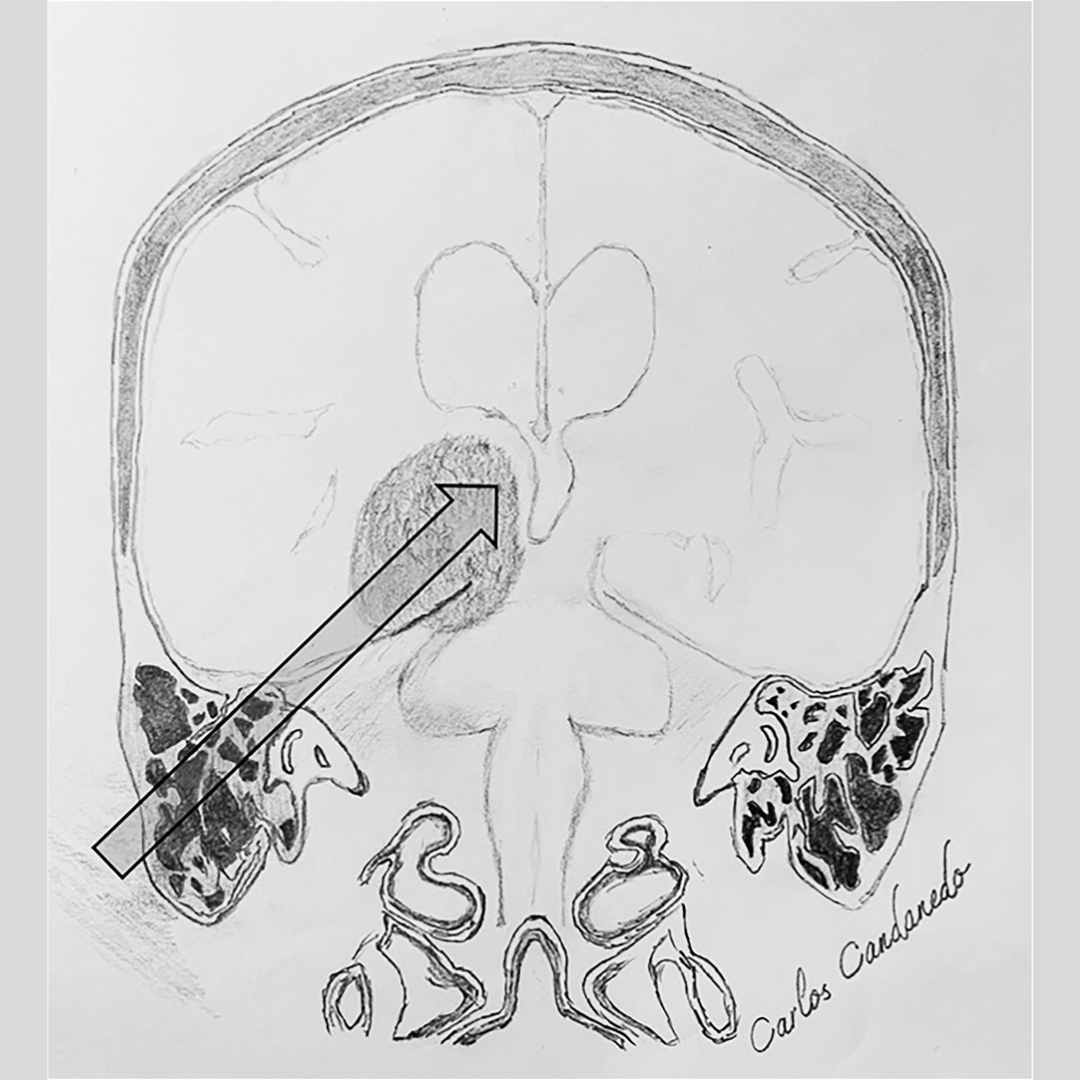
Results: During the study period, 32 posterior fossa HGBs were resected. There were 26 cerebellar lesions, 4 medullary lesions, and in 2 patients, both structures were affected. Predominantly cystic tumors were seen in 15 patients and solid tumors in 17. Preoperative digital subtraction angiography (DSA) was performed in 8 patients with solid tumors, and 4 showed tumor-related aneurysms. Embolization of the tumors was performed in 6 patients, including the four tumor-related aneurysms. GTR was achieved in 29 tumors (91%), and subtotal resection in 3 (9%). Three patients had postoperative lower cranial nerve palsy. Functional status was stable in 5 patients (16%), improved in 24 (75%), and 3 patients (9%) deteriorated. One patient died 2 months after surgery. Two tumors recurred and underwent a second surgery, achieving GTR. The mean follow-up was 42.7 months (SD ± 51.0 months).
Conclusions: Predominantly cystic HGB is usually easily treated as the surgery is straightforward. Those with solid predominance present a more complex challenge, sharing features similar to arteriovenous malformations. Given the important vascular association of solid predominance HGB with these added risk factors, the preoperative assessment should include DSA, as in arteriovenous malformations, and endovascular intervention should be considered before surgery.