The infratranstentorial subtemporal approach (ITSTA): a valuable skull base approach to deep-seated non-skull base pathology
Carlos Candanedo, Samuel Moscovici, Sergey Spektor
Received: 11 May 2019 / Accepted: 22 August 2019 / Springer-Verlag GmbH Austria, part of Springer Nature 2019
Abstract
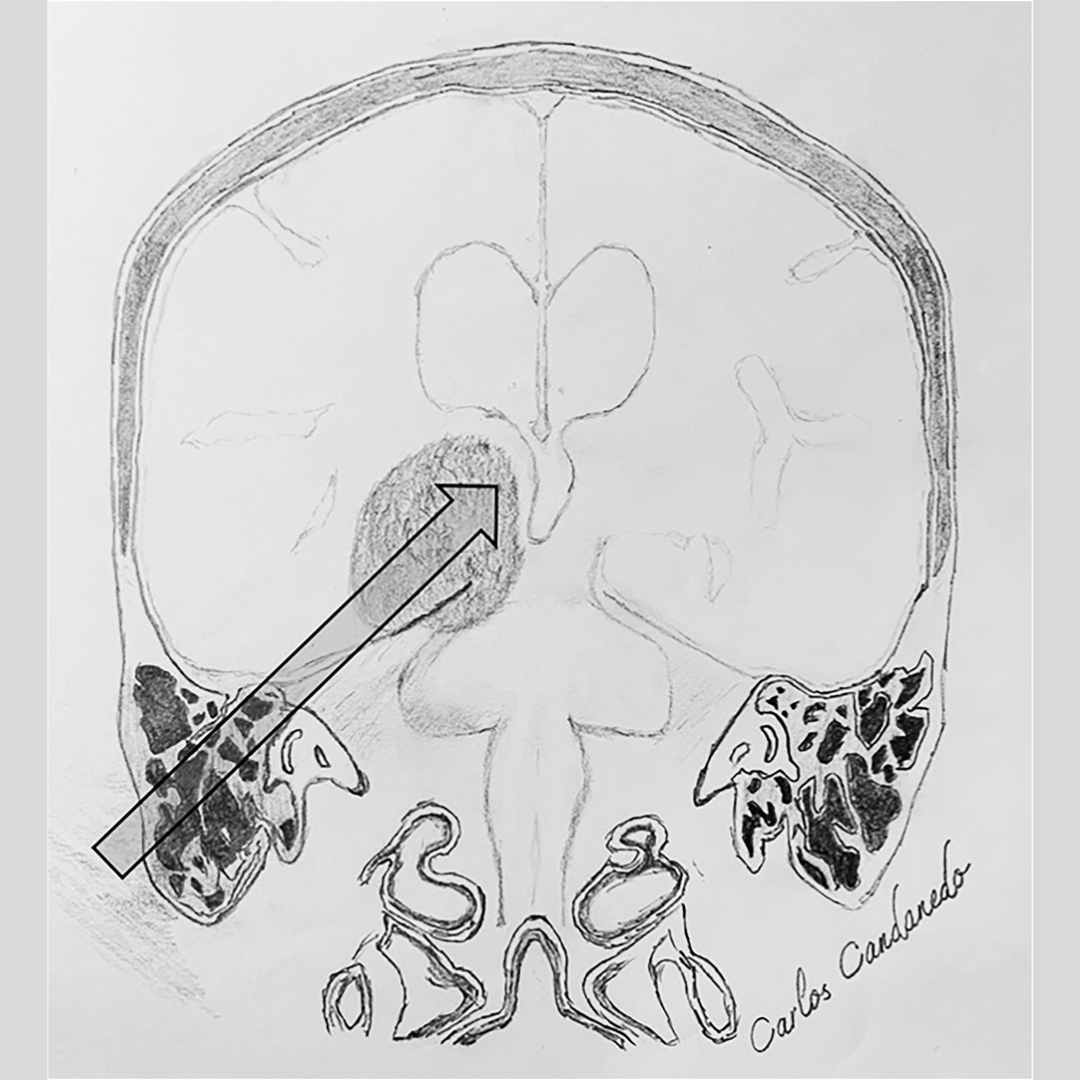
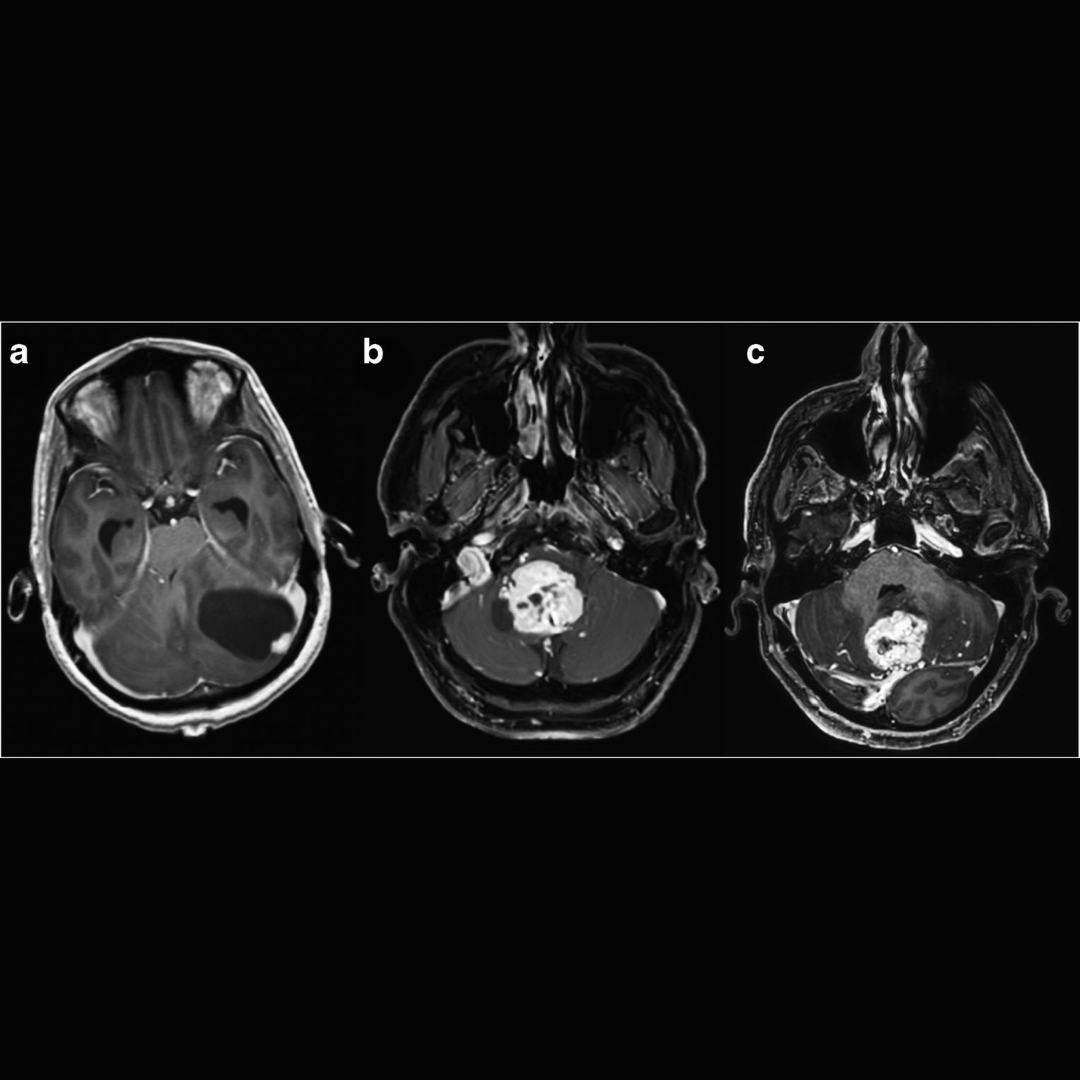
Background: Surgical access to space-occupying lesions such as tumors and vascular malformations located in the area of the tentorial notch, mediobasal temporal lobe, and para-midbrain is difficult. Lesions in this area are typically resected with supratentorial approaches demanding significant elevation of the temporal lobe or even partial lobectomy, or via a supracerebellar transtentorial approach. We introduce an alternative, the skull base infratranstentorial subtemporal approach (ITSTA), which provides excellent exposure of the incisural area while minimizing risk to the temporal lobe.
Methods: We included consecutive patients with pathology involving the area of the tentorial incisura, para-midbrain, and mediobasal temporal area who underwent surgery via ITSTA from 2012 to 2018. The approach includes partial mastoidectomy, temporal craniotomy, and tentorial section. Space obtained by mastoidectomy provides a sharp high-rising angle-of-attack, significantly diminishing the need for temporal lobe retraction. Surgeries were performed using microsurgical techniques, neuronavigation, and electrophysiological monitoring. Clinical presentation, tumor characteristics, extent of resection, complications, and outcome were retrospectively reviewed under a waiver of informed consent.
Results: Nine patients met inclusion criteria (five female, four male; mean age 44 years, range 7–72). They underwent surgery for removal of para-midbrain arteriovenous malformation (AVM, 3/9), medial tentorial meningioma (2/9), mediobasal epidermoid cyst (2/9), oculomotor schwannoma (1/9), or pleomorphic xanthoastrocytoma (PXA) of the fusiform gyrus (1/9). Three AVMs were removed completely; among six patients with tumors, gross total resection was achieved in three and subtotal resection in three. All surgeries were uneventful without complications. There were no new permanent neurological deficits. At late follow-up (mean 42.5 months), eight patients had a Glasgow Outcome Score (GOS) of 5. One 66-year-old female died 18 months after surgery for reasons not related to her disease or surgery.
Conclusions: The ITSTA is a valuable skull base approach for removal of non-skull base pathologies located in the difficult tentorial-incisural parabrainstem area.
Keywords
Arteriovenous malformation, Incisura, Skull base, Subtemporal, Tentorial notch, Transtentorial